Abstract
Background. Donor specific antibodies (DSAs) are preformed IgG antibodies with specificity against HLA molecules not shared with the donor that can lead to graft failure (GF) in the setting of mismatched HSCT. The aim of this study is to report the experience of the Spanish Group of Hematopoietic Transplant (GETH-TC) in patients with DSAs undergoing haplo-HSCT.
Methods. Patients undergoing haplo-HSCT in centers from the GETH-TC from 2013 to 2021 were included in the study. DSAs were analyzed with a solid-phase single-antigen immunoassay (Luminex®); monitoring was performed prior to desensitization, prior to infusion and after infusion. Desensitization strategies used depended on center experience, immunofluorescence intensity, complement fixation and type of antibodies.
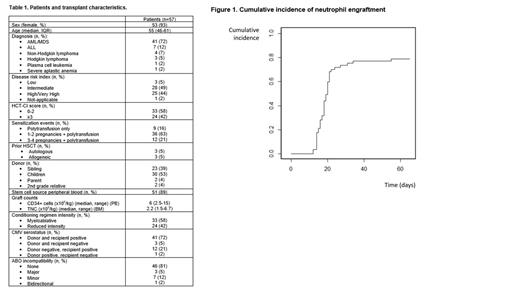
Results. 59 haplo-HSCT with DSAs were performed in 57 patients in 13 centers. Characteristics of the population are shown in Table 1. 53 (93%) patients were female (91% with prior pregnancies). All patients lacked a suitable alternative donor. 51 (89%) received peripheral blood as stem cell source. Conditioning was myeloablative in 58% and all patients received post-transplant cyclophosphamide based GVHD prophylaxis; 3 (5%) patients received also ATG.
28 (49%) patients presented anti-HLA class I DSAs 22 of them with >5000MFI), 14 (25%) presented anti-HLA class II (6 with >5000MFI) and 15 (26%) presented both anti-HLA class I and II DSAs (13 with >5000MFI). Five patients did not receive desensitization treatment, 4 of them with <5000MFI. Of 52 patients receiving desensitization treatment, 49 received at least two treatments as desensitization strategy and all but 3 (6%) experienced a decrease of MFI after desensitization (mean reduction 80%); 2 out of those 3 patients developed GF. Desensitization treatments used included RTX in 83% of patients, IVIG (65%), therapeutic plasma exchange (TPE) (60%), incompatible platelets (16%), MMF (42%), buffy coat (only in patients with class II DSAs, 23%), tacrolimus (21%), bortezomib (4%) and steroids (2%). Cumulative incidence of neutrophil engraftment at day 30 was 74% (Figure 1), in a median of 18 days (IQR, 15-20); five patients died before engraftment due to toxicity and 7 patients experienced primary GF despite desensitization in 6 of them. 4 of them received a 2 nd transplant, one was alive after day 100. 30 (53%) patients died during the study period: 6 due to GF, 7 due to relapse, 7 due to infection, 6 due to endothelial complications (SOS, TA-TMA and diffuse alveolar hemorrhage) and 4 because of GVHD.
After a median follow-up of 24 months, 2-year OS and EFS were 52% and 42%, respectively. 2-year cumulative incidence of relapse at was 14% and NRM was 41%. Cumulative incidence of grade II-IV aGVHD at day 180 was 13% and chronic GVHD was 25%.
Conclusions. The use of desensitization treatment guided by DSAs intensity kinetics constitute an effective approach with high rates of engraftment for patients with DSAs in need for an haplo-HSCT lacking an alternative suitable donor, including non-malignant disorders.
Bailen: Pfizer, Kite-Gilead, Gilead: Honoraria. Oarbeascoa: Gilead: Honoraria, Speakers Bureau. Kwon: Novartis, Celgene, Gilead, Pfizer: Consultancy, Honoraria.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal